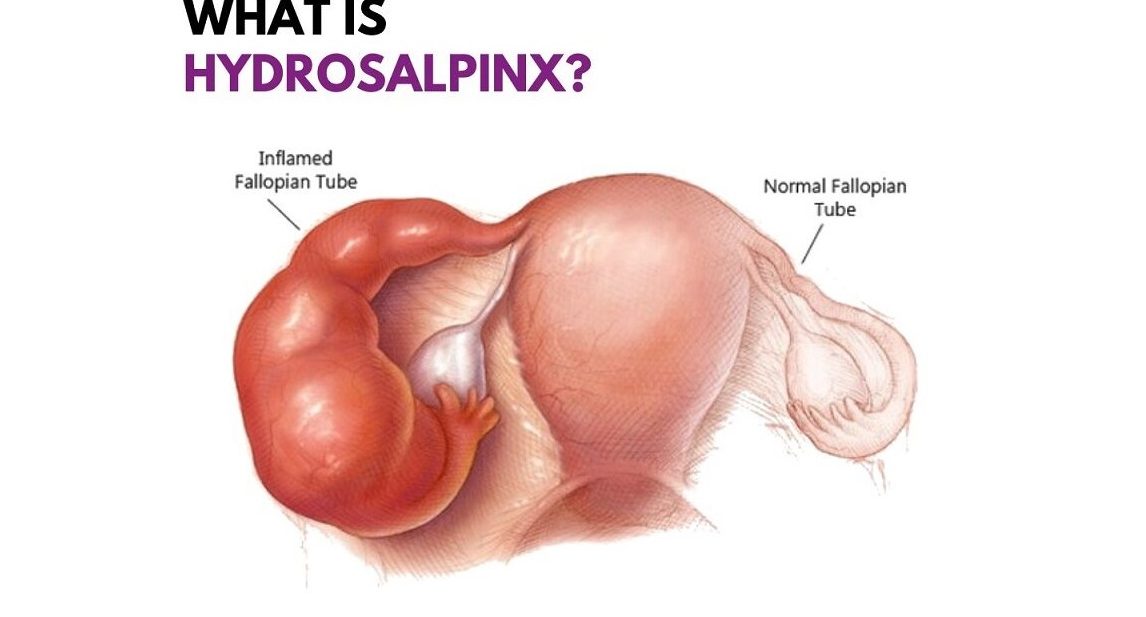
What is Salpingectomy for Hydrosalpinx?
Symptoms of Hydrosalpinx
Many women with hydrosalpinx do not experience noticeable symptoms. However, some may face:
- Pelvic pain or discomfort
- Lower abdominal pain
- Unusual vaginal discharge
- Infertility or difficulty conceiving
- Pain during intercourse
Since it often remains silent, it is usually diagnosed during fertility evaluations or ultrasound scans prior to IVF treatment.
Procedure or Treatment
1. Pre-operative Preparation:
Diagnosis through ultrasound or HSG (Hysterosalpingography).
Blood tests and pre-anesthesia evaluations.
2. Surgical Procedure:
Performed under general anesthesia.
Mostly done laparoscopically (keyhole surgery) for minimal invasiveness.
The affected fallopian tube is carefully separated from surrounding tissues and removed.
The ovaries and uterus are left intact to proceed with IVF treatment.
3. Recovery:
Usually discharged within 24-48 hours.
Return to daily activities within a week.
Advised to avoid heavy lifting and strenuous work for a few weeks.
Prevention
Hydrosalpinx cannot always be prevented, but reducing the risk of sexually transmitted infections (STIs) and pelvic inflammatory disease (PID) can help. Preventive measures include:
- Practicing safe sex
- Seeking early treatment for infections
- Regular gynecological check-ups
Benefits of Salpingectomy Before IVF
- Improves IVF Success Rates: Removes toxic fluid that can harm embryos.
- Reduces Risk of Infection: Eliminates the diseased tube, lowering chances of infection spreading.
- Prevents Ectopic Pregnancy: Blocks risk of ectopic pregnancies in a damaged tube.
- Enhances Uterine Environment: Provides a healthier environment for embryo implantation and growth.
- Permanent Solution: Once the tube is removed, recurrence of hydrosalpinx is eliminated in that tube.
Types of Salpingectomy
Unilateral Salpingectomy
Removal of one fallopian tube.
Common when hydrosalpinx is present only on one side.
Bilateral Salpingectomy
Removal of both fallopian tubes.
Sometimes done if both tubes are severely damaged or blocked.
Partial Salpingectomy (Salpingostomy)
Only a part of the tube is removed or opened.
Less commonly used for hydrosalpinx before IVF due to risk of fluid reaccumulation.
Laparoscopic Salpingectomy
Minimally invasive approach with small incisions.
Faster recovery, less pain, and minimal scarring.
Open Salpingectomy
Traditional open surgery with a larger incision.
Rarely required unless there are extensive adhesions or other complications.
