What is Splenectomy and Splenic Salvage?
Symptoms That May Indicate the Need for Splenectomy
Splenectomy or splenic salvage may be considered if the patient experiences:
- Frequent infections or sepsis due to spleen dysfunction
- Chronic or severe pain in the upper left abdomen
- Fatigue or anemia
- Unexplained weight loss
- Low platelet or red blood cell count (due to splenic sequestration)
- Enlarged spleen (splenomegaly) causing pressure on surrounding organs
- Trauma to the spleen causing internal bleeding
Common Conditions That May Require a Splenectomy or Splenic Salvage
- Splenic rupture (due to accident or trauma)
- Hematologic diseases like idiopathic thrombocytopenic purpura (ITP), sickle cell anemia, or hereditary spherocytosis
- Certain cancers, including lymphoma or leukemia
- Abscess, cyst, or tumors of the spleen
- Hypersplenism (overactive spleen)
- Autoimmune disorders
Procedure / Treatment
1. Splenectomy
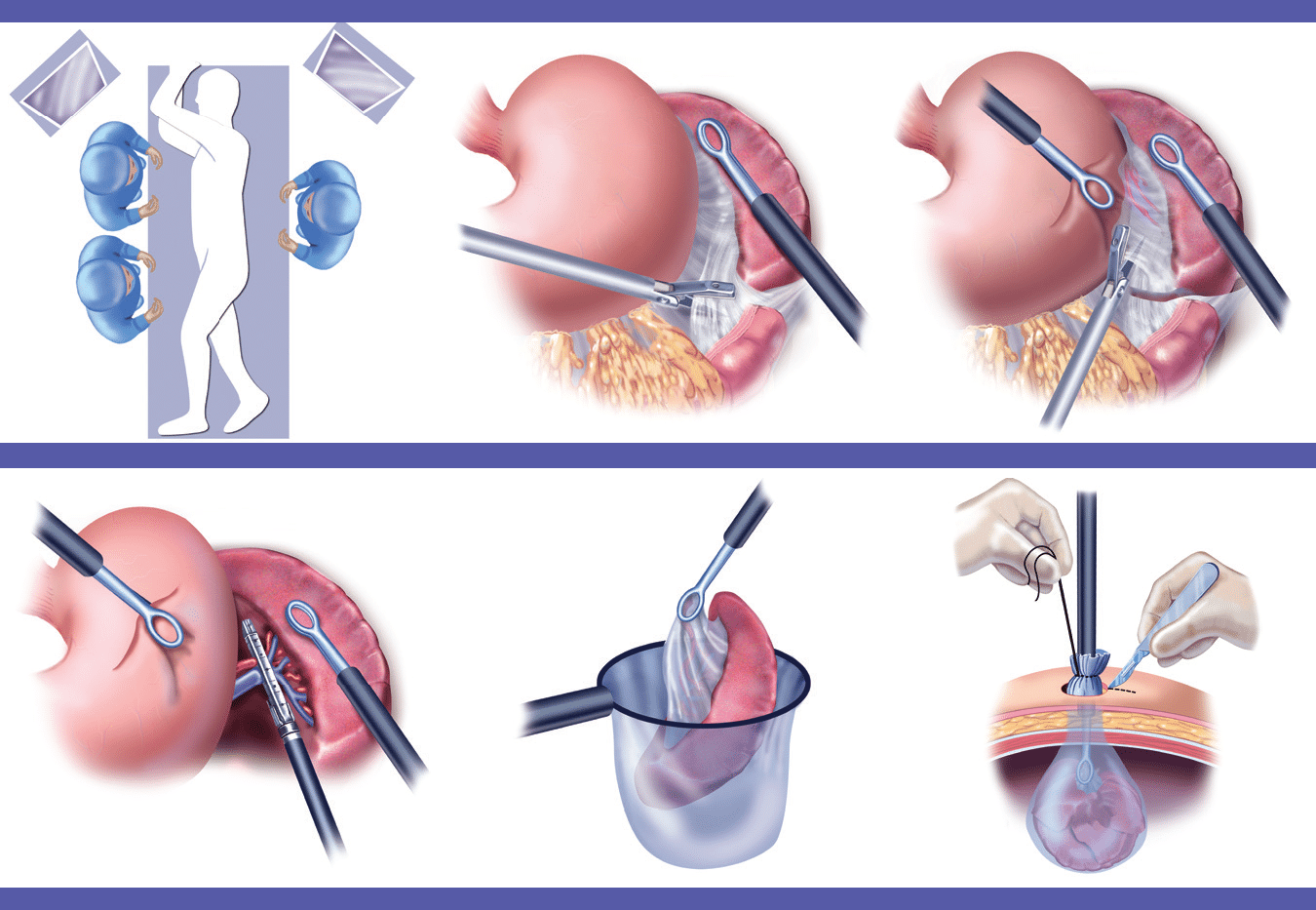
Splenectomy can be performed using:
Laparoscopic surgery (minimally invasive): Involves small incisions, faster recovery, and less postoperative pain.
Open surgery: Used in emergencies or if the spleen is significantly enlarged or damaged.
The patient is usually given general anesthesia. The surgeon removes the spleen, controls bleeding, and closes the incision. Postoperative care includes vaccinations and antibiotics to prevent infections.
2. Splenic Salvage Procedures
These include:
Partial splenectomy: Only the damaged part is removed.
Splenorrhaphy: Surgical repair of the spleen using sutures, mesh, or topical agents.
Embolization: Blocking blood flow to a part of the spleen to stop bleeding or reduce its size without removal.
These procedures aim to maintain immune function and reduce the risk of life-long infections associated with total splenectomy.
Prevention and Postoperative Care
While some spleen issues are not preventable (especially trauma), managing underlying diseases early can reduce risks. After splenectomy:
Vaccinations (against pneumococcus, meningococcus, and Haemophilus influenzae) are crucial before or shortly after surgery.
Antibiotics may be prescribed for several months post-surgery or longer in children.
Regular follow-ups are important to monitor blood counts and immune function.
Benefits of Splenectomy and Splenic Salvage
- Relief from chronic pain or symptoms caused by spleen disorders
- Prevention of life-threatening internal bleeding
- Improved blood count levels in patients with hematologic disorders
- Preservation of immune function through splenic salvage
- Reduced risk of postoperative complications with laparoscopic techniques
