What is Haemorrhoidectomy?
Haemorrhoidectomy is a surgical procedure performed to remove severe or prolapsed haemorrhoids (piles) that cause pain, bleeding, or discomfort. Haemorrhoids are swollen veins in the lower rectum or anus, often resulting from straining during bowel movements, chronic constipation, or prolonged sitting. When non-surgical treatments like dietary changes, medications, or minimally invasive procedures fail, a haemorrhoidectomy is often recommended for long-term relief.
There are two main types of haemorrhoidectomy:
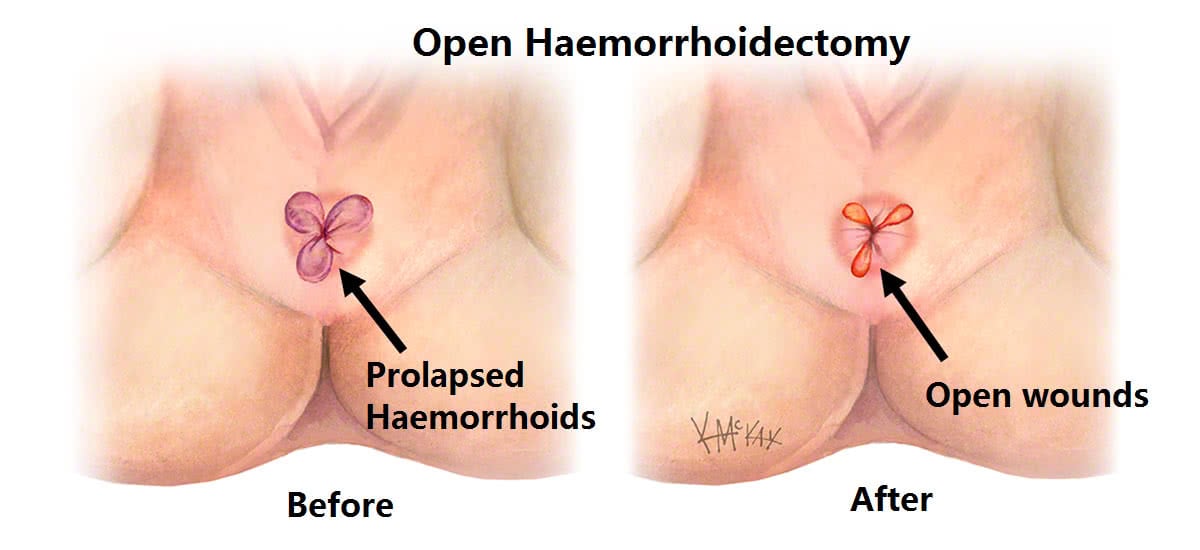
Open Haemorrhoidectomy: The haemorrhoid is surgically removed, and the wound is left open to heal naturally.
Stapled Haemorrhoidopexy (PPH): A surgical stapling dev
Symptoms of Haemorrhoids
Common symptoms that may indicate the need for surgery include:
- Bright red bleeding during bowel movements
- Pain or discomfort in the anal region
- Itching or irritation around the anus
- Swelling or a lump near the anus
- Mucus discharge or soiling
- Difficulty sitting for prolonged periods
- Prolapsed haemorrhoids that do not retract
Surgical Procedure & Treatment
Open Haemorrhoidectomy:
Performed under spinal or general anaesthesia.
The surgeon excises the haemorrhoidal tissue using a scalpel or laser.
The area may be left open (open technique) or stitched closed (closed technique).
Healing typically takes 2–4 weeks.
Stapled Haemorrhoidopexy:
Less painful alternative for internal haemorrhoids.
Involves a circular stapling device that cuts off the blood supply and repositions the haemorrhoidal tissue.
Minimal incisions, less post-operative discomfort, and faster recovery.
Suitable for Grade III and IV internal haemorrhoids.
Types of Haemorrhoidectomy
- Open Haemorrhoidectomy
- Closed Haemorrhoidectomy
- Stapled Haemorrhoidopexy (PPH)
- Laser Haemorrhoidectomy (advanced option, less invasive)
- Doppler-Guided Haemorrhoidectomy (targeted technique using ultrasound guidance)
Prevention of Haemorrhoid
While surgery addresses existing haemorrhoids, adopting preventive measures can help reduce recurrence:
- Increase fiber intake (fruits, vegetables, whole grains)
- Stay hydrated
- Avoid straining during bowel movements
- Exercise regularly to prevent constipation
- Avoid sitting for prolonged periods, especially on the toilet
- Maintain a healthy weight
Benefits of Haemorrhoidectomy Surgery
- Long-term relief from painful and bleeding haemorrhoids
- Effective for advanced-stage piles
- Reduced risk of recurrence
- Improved quality of life
- Stapled method offers quicker recovery and less pain
