What is Neck Dissection?
Symptoms Indicating Neck Dissection May Be Needed
Patients with thyroid cancer may experience:
- Swelling or lump in the neck
- Enlarged lymph nodes
- Hoarseness of voice
- Difficulty swallowing
- Persistent throat pain
- Changes in breathing
- Cough not related to cold
If cancer spreads to lymph nodes, these symptoms may worsen or new lumps may appear in the neck.
Procedure / Treatment
Preoperative Evaluation:
- Ultrasound neck
- Fine needle aspiration cytology (FNAC) of suspicious lymph nodes
- CT or MRI if required
During Surgery:
Performed under general anesthesia
Incision is made along natural neck creases for minimal visible scarring
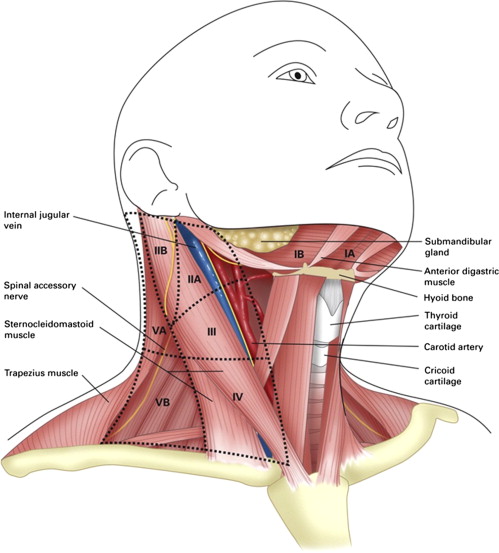
Removal of lymph nodes in specific neck compartments (levels I-VI) depending on cancer spread
Types include:
Central neck dissection (Level VI): for nodes near thyroid
Lateral neck dissection (Levels II-V): for spread to side neck nodes
Selective neck dissection: removes only specific lymph node groups
Modified radical neck dissection: removes lymph nodes with preservation of key structures like nerves and muscles
Radical neck dissection: removes all lymph nodes along with sternocleidomastoid muscle, internal jugular vein, and spinal accessory nerve (rarely required now)
Postoperative Care
- Hospital stay of 2-3 days
- Drain removal within 48 hours
- Pain management and antibiotics
- Monitoring for complications like nerve injury or hypocalcemia
- Follow-up with oncologist or endocrine surgeon for further treatment like radioactive iodine therapy if needed
Prevention
While neck dissection itself is a treatment, prevention of lymph node spread includes:
Early detection and treatment of thyroid cancer
Regular neck ultrasound in known thyroid malignancy patients
Fine needle aspiration of suspicious lymph nodes for early intervention
Benefits of Neck Dissection
Removes cancerous lymph nodes, reducing risk of recurrence
Improves long-term survival rates
Provides accurate cancer staging to guide further treatment
May improve cosmetic outcomes by preventing visible nodal swelling
Increases chances of complete cancer removal when combined with thyroidectomy
Types of Neck Dissection
Central Neck Dissection (Level VI)
Removes lymph nodes between carotid arteries and from hyoid bone to sternal notch
Lateral Neck Dissection (Levels II-V)
Removes nodes along side of the neck where cancer often spreads
Selective Neck Dissection
Only specific lymph node groups removed based on cancer spread pattern
Modified Radical Neck Dissection
Removes lymph nodes and surrounding fat while preserving key nerves and muscles for better function
Radical Neck Dissection
Extensive removal including muscles, veins, and nerves (rarely used now due to advanced targeted approaches)
